You'll usually be admitted to hospital on the day of your operation. The surgeon and anaesthetist will usually come and see you to discuss what will happen and answer any questions you have.
Most people would have seen their surgeon at a pre-assessment clinic and had the chance to discuss any relevant details of the operation.
A senior-level surgeon, consultant or registrar will perform surgery. They may be helped by junior doctors. You should be told at your pre-operative assessment who will be doing the operation. If you're not told, don't be afraid to ask.
How the operation is carried out
Knee replacement surgery is usually performed either under general anaesthetic (you're asleep throughout the procedure) or under spinal or epidural anaesthetic (you're awake but have no feeling from the waist down).
The worn ends of the bones in your knee joint are removed and replaced with metal and plastic parts (a prosthesis) which have been measured to fit.
You may have either a total or a half-knee replacement. This will depend on how damaged your knee is. Total knee replacements are the most common.
Read more information about what happens on the day of your operation.
Total knee replacement
In a total knee replacement (TKR), both sides of your knee joint are replaced. The procedure takes one to three hours:
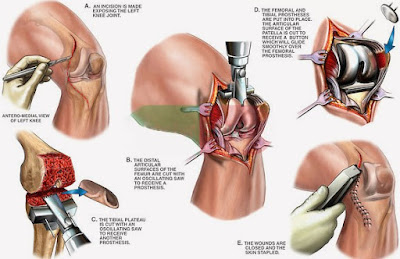
- Your surgeon makes a cut down the front of your knee to expose your kneecap. This is then moved to the side so the surgeon can get to the knee joint behind it.
- The damaged ends of your thigh bone (femur) and shin bone (tibia) are carefully cut away. The ends are precisely measured and shaped to fit the appropriately sized prosthetic replacement. A dummy joint is positioned to test that the joint is working properly. Adjustments are made, the bone ends are cleaned, and the final prosthesis is fitted.
- The end of your femur is replaced by a curved piece of metal, and the end of your tibia is replaced by a flat metal plate. These are fixed using special bone 'cement', or are treated to encourage your bone to fuse with the replacement parts. A plastic spacer is placed between the pieces of metal. This acts like cartilage, reducing friction as your joint moves.
- The back of the knee cap may also be replaced, depending on the reasons for replacement.
- The wound is closed with either stitches or clips and a dressing is applied to the wound. In rare cases a splint is used to keep your leg immobile, but you're usually encouraged to move your knee as early as possible.
Total knee replacement is a common procedure but you're still likely to have some difficulty moving, especially bending your knee, and kneeling may be difficult because of the scar.
Partial (half) knee replacement
If only one side of your knee is damaged, you may be able to have a partial (half) knee replacement (PKR). PKR is a smaller operation, which uses a smaller incision, and involves less bone being removed. It's suitable for around one in four people with osteoarthritis.
There are advantages to PKR including a shorter hospital stay and recovery period. Blood transfusions are also rarely needed. PKR often results in more natural movement in the knee and you may be able to be more active than after a total knee replacement.
Talk to your surgeon about the type of surgery they intend to use and why they think it's the best choice for you.
Other procedures
In some cases, there may be other types of procedure used, including:
Kneecap replacement
If only your kneecap is damaged, an operation called a patellofemoral replacement or patellofemoral joint arthroplasty can be performed. This involves a smaller surgery with a faster recovery time. However, the long-term results are still unclear and it's not suitable for most people with osteoarthritis.
Mini-incision surgery (MIS)
This new technique has been recommended by the National Institute for Health and Care Excellence (NICE). It can be used for either total or half knee replacements, but is currently more commonly used for half knee replacements.
The surgeon makes a smaller cut than in standard knee replacement surgery. Specialised instruments are then used to manoeuvre around the tissue, rather than cutting through it. This should lead to a quicker recovery.
Read the NICE guidance on mini-incision surgery for total knee replacement.
Image-guided surgery
The surgeon performs this operation using computerised images, which are generated by attaching infrared beacons to parts of your leg and to the operating tools. These are tracked on infrared cameras in the operating theatre. Results so far suggest that this may enable the new knee joint to be positioned more accurately.
Most hospitals don't yet have the equipment to do this and only around 1% of knee replacements are performed in this way.
Patient-specific knee replacement
This is a more recent advance in knee replacement surgery. A guide is created using magnetic resonance imaging (MRI) scans. This helps to create the best fitting implant for each patient.
The potential advantage of this procedure is that the implant may last longer, as the most accurate fitting is used. However, as this is a new technique, the results and long-term effects aren't fully known yet.